
Heroin. Alluring and dangerous. This white (or sometimes brown) powder, usually melted by heat and injected intravenously, is used by more than 17 million people worldwide.
The narcotic heroin is made from morphine, which is derived from the flowering opium poppy plant. In America, nearly 80 percent of heroin addicts start out by taking prescription painkillers like Vicodin and Oxycontin. Given the current opioid epidemic plaguing the U.S., it’s no wonder more and more people are wisely seeking out heroin addiction treatment centers.
Dangers of Heroin Use and Why Recovery Is Challenging
Heroin is highly addictive. When injected into a vein, it hits the opioid receptors in the brain quickly and has 2 to 3 times the effect of a similar dose of morphine. Because of these factors and the euphoric feelings of pleasure the drug emits, heroin addiction is tough to break.
Prolonged heroin use can cause:
- Abscesses (pus-filled boils on the skin)
- Stomach problems
- Liver and kidney disease
- Mental disorders
- Sexual problems
- Risk of HIV, hepatitis and other bloodborne diseases
- Permanent brain damage
- Decreased ability to breathe
While there are many additional health risks of using heroin and other opioids, the most disturbing one is overdose and death. Due to impaired judgment and the severe withdrawal distress that occurs within hours of last use, accidental overdose happens all too frequently. If the user does not receive emergency help immediately, death is often the result.
According to the National Institute on Drug Abuse, the number of Americans dying from illicit opioid overdose is approaching 25,000 annually. And while there is a significant reason for heroin users to seek treatment, the individual must really want help and be self-motivated for any treatment to work.
Heroin Addiction Treatment Success Rates
Heroin addiction is tough. You have to be tougher. You have to want to get clean.
People will not perform behaviors unless or until they are motivated to do so. Studies reveal the more people are motivated to change, the more successful they will be with the desired change. The patient’s level of motivation, an important factor in success rates in addiction treatment, contributes significantly to the effectiveness of interventions, therapy and rehab.
People in recovery who have some motivating reasons to get well have a lower attrition rate than those people who are not self-motivated.
If you truly want to be successful and are ready to become sober for good, the Maryland Recovery heroin treatment programs can be your best chance at achieving a lasting recovery from heroin addiction.
The Recovery Homes at Maryland Recovery
Recovery homes subscribe to a social model approach to rehab. Individuals in our outpatient programs learn life skills during treatment and live in a recovery home, thereby receiving an immersive rehabilitation experience.
There are many benefits of staying in a recovery home while undergoing drug rehab. Here are a few of the advantages:
- Recovery homes are less expensive than inpatient programs.
- Clients can go to work and attend school while in rehab.
- Most people are more comfortable in a home-like environment than a hospital.
- Clients can still receive intensive treatment for addiction with more freedom than inpatient care.
- Residents have numerous opportunities to engage socially with others going through similar sobriety work.
- Support groups and meetings are easily accessible.
- Accountability checks keep residents on track with a curfew, housework contribution to community living, and the commitment to staying drug-free.
Clients involved in Maryland Recovery housing participate in our intensive outpatient program and partial hospitalization programs housed in our outpatient facility in downtown Bel Air, MD.
Intensive Outpatient Heroin Program
For individuals wanting to successfully quit heroin for good, an intensive outpatient program (IOP) can be the best answer. Oftentimes, insurance doesn’t cover long hospital and inpatient stays, leaving the patient unready to face the challenges of acclimating to a new drug-free life. People struggling with heroin addiction can instead choose a long-term IOP.
The treatment options in an IOP include:
- Group and individual therapy
- Family education and therapy
- Relapse prevention and life skill building
- Tools for dealing with cravings and triggers
- 12-step meetings
A heroin addiction rehab center shouldn’t offer treatment for a pre-set number of days, but often that is the case. Thirty, 60, or 90 days might work for some people, but we are all unique individuals and when it comes to addiction recovery, you want a drug abuse treatment center that caters to your specific needs.
At Maryland Recovery, we have no set time that you must be healthy by. The decision on when it complete rehab is in your hands.
Recovery Housing Coupled with an Intensive Outpatient Program
There is a multitude of advantages in participating in a program that offers both a recovery home and effective outpatient rehabilitation. Relapse prevention, better recovery skills and a support system highlight a few such advantages.
Relapse Prevention
Lengthy education, day-to-day structure, and help in implementing a new lifestyle work together to minimize your risk of going back to heroin.
Better Recovery Skills
Imagine a longer time frame to work on honing your new addiction-fighting skills. It’s easy to see how practicing new behaviors for a lengthier period of time aids in mastery.
Support System
Research has taught us the value of a support system when it comes to addiction recovery. And when you live with people, you inevitably become close. Gaining this new circle of supportive friends who know firsthand what you’re up against offers you the chance of a lifelong support system and some great future accountability partners and sponsors.
Holistic Rehab Approach
There are reasons we as humans develop addictions. At Maryland Recovery, our goal is to help people understand their personal reasons and to heal mentally, physically and spiritually.
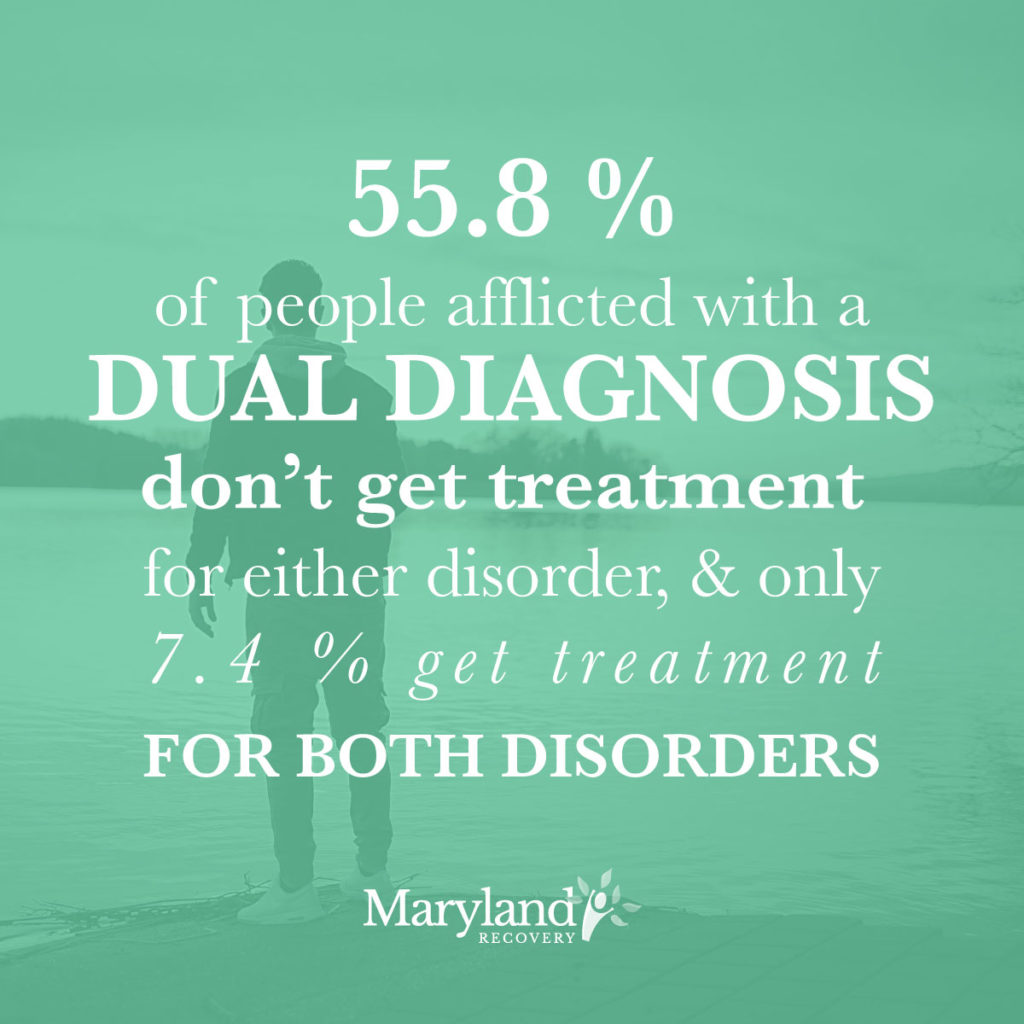
We believe in recovery for the whole person. That’s why we are one of the leading dual diagnosis treatment centers on the East Coast. We understand that mental illness and drug addiction go hand in hand; statistics bear it out. Whether someone uses heroin to mask the pain of mental illness or they develop a mental illness because of heavy heroin use, we are here to help them attain complete wellness.
Maryland Recovery
If you are looking for the answer to successfully beat heroin addiction, our outpatient program-recovery home model might be perfect for you. The benefits of recovery housing coupled with a holistic intensive outpatient program can be a tremendous advantage in starting a journey to lasting sobriety.
Admitting you have a problem and need help is the first step. And the first step in learning what we can offer you personally begins with that first contact.
Heroin addiction is tough. Be tougher. Contact Maryland Recovery today.
Learn About Us and Our Recovery Homes
The post Finding Heroin Addiction Treatment Success with Maryland Recovery appeared first on Maryland Recovery.



 During and after recovery from an addiction, support groups are necessary. Support groups give those recovering from addiction a formal support system. Active participation in these groups can reduce the rate of relapse and encourage commitment to recovery. Group members provide support and friendship to others who have suffered from the same addictions. Group members encourage sobriety and work to keep others on track.
During and after recovery from an addiction, support groups are necessary. Support groups give those recovering from addiction a formal support system. Active participation in these groups can reduce the rate of relapse and encourage commitment to recovery. Group members provide support and friendship to others who have suffered from the same addictions. Group members encourage sobriety and work to keep others on track.




 It’s not uncommon for individuals to develop depression during the recovery process, which can be an especially troubling experience. After all, making the decision to get sober is a good thing, so it doesn’t make much sense when the person feels worse about themselves than they did before.
It’s not uncommon for individuals to develop depression during the recovery process, which can be an especially troubling experience. After all, making the decision to get sober is a good thing, so it doesn’t make much sense when the person feels worse about themselves than they did before.

 alcohol isn’t easy. Understanding that a problem exists is the first step to solving that problem.
alcohol isn’t easy. Understanding that a problem exists is the first step to solving that problem.








 Finding a dual diagnosis treatment program that includes therapy for both conditions is important. Many rehabilitation facilities are not capable of handling dual diagnosis patients. Therapy for simultaneous treatment of both diagnoses is still a relatively new concept.
Finding a dual diagnosis treatment program that includes therapy for both conditions is important. Many rehabilitation facilities are not capable of handling dual diagnosis patients. Therapy for simultaneous treatment of both diagnoses is still a relatively new concept.

 In many cases, people develop agoraphobia because of a traumatic event, and they fear it will happen again in a similar circumstance. For instance, people who experience a panic attack in public will begin to fear it will repeat itself, and thus exhibit avoidance behaviors.
In many cases, people develop agoraphobia because of a traumatic event, and they fear it will happen again in a similar circumstance. For instance, people who experience a panic attack in public will begin to fear it will repeat itself, and thus exhibit avoidance behaviors.



 DEA officers and Dr. Kathryn Hawk of Yale New Haven Hospital confirmed emergency crews’ suspicions that opioids were involved. In at least one sample, they found that K2 “spice” – a form of synthetic marijuana – had been mixed with fentanyl, a powerful synthetic opioid.
DEA officers and Dr. Kathryn Hawk of Yale New Haven Hospital confirmed emergency crews’ suspicions that opioids were involved. In at least one sample, they found that K2 “spice” – a form of synthetic marijuana – had been mixed with fentanyl, a powerful synthetic opioid.

 Underlying conditions as dual diagnosis can include any of the following:
Underlying conditions as dual diagnosis can include any of the following:





 Before administering Narcan capriciously, check for the signs of overdose before moving forward. Possible signs of opioid overdose include:
Before administering Narcan capriciously, check for the signs of overdose before moving forward. Possible signs of opioid overdose include:
 Researchers at McGill University in Montreal Canada took a
Researchers at McGill University in Montreal Canada took a 
 Some people avoid medication because accepting a prescription means admitting to having a disorder. There is an unfortunate stigma surrounding mental illness and chronic medical conditions that causes some people to feel ashamed of these issues. Some people may want to overcome addiction without relying on foreign substances in the body, but may not realize that a co-occurring condition is a major part of the problem and it requires treatment.
Some people avoid medication because accepting a prescription means admitting to having a disorder. There is an unfortunate stigma surrounding mental illness and chronic medical conditions that causes some people to feel ashamed of these issues. Some people may want to overcome addiction without relying on foreign substances in the body, but may not realize that a co-occurring condition is a major part of the problem and it requires treatment.







